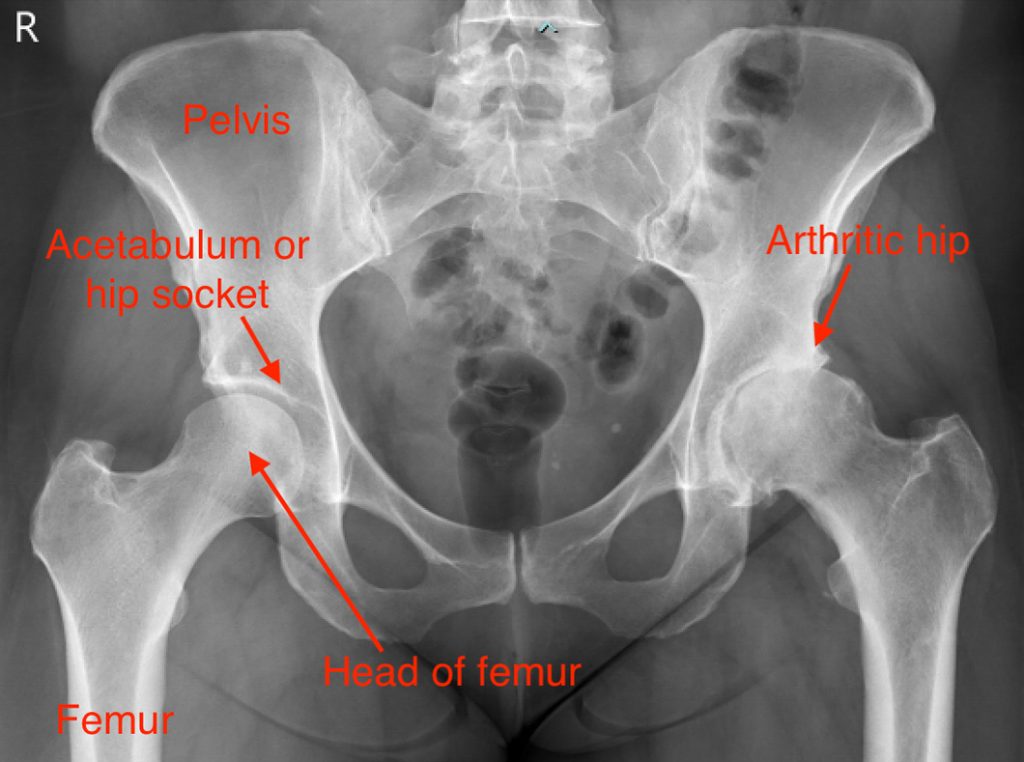
HIP ARTHRITIS
The hip joint is one of the common joints affected by arthritis. Because it is a major weight-bearing joint with an essential role in many activities, it can have a significant impact on your life. Arthritis is a slowly progressive disease that progresses over years to decades. When the cartilage is entirely lost, you may reach the stage of having “bone on bone”.
Many conditions lead to cartilage damage and osteoarthritis. However, most cases are idiopathic, which means that there is no specific cause. There is probably a genetic component to this idiopathic variety, and joints other than the hip are commonly involved (knee and hand). Another cause of hip arthritis, particularly in younger patients, is hip dysplasia. Fractures around the hip joint and femoroacetabular impingement can lead to cartilage damage. There is some evidence that long-term repetitive trauma can also impact on the hip. Diseases that cause inflammation of a joint such as Rheumatoid Arthritis can lead to cartilage damage. Arthritis is more common as we age, but it is not an inevitable consequence of ageing. Finally, there is evidence that obesity may have a primary role in the development of arthritis as well as placing an increased load through the joint.

The predominant symptom of arthritis is pain. The discomfort is usually felt in the groin and may radiate into the thigh. Often the pain from osteoarthritis is intermittent.
Call us on (03) 5223 3151 Book an appointment today.
SYMPTOMS
The predominant symptom of arthritis is pain. The discomfort is usually felt in the groin and may radiate into the thigh. Often the pain from osteoarthritis is intermittent. Factors such as increased activity (e.g. going for a much longer walk than usual) or a minor injury may trigger an acute exacerbation.
Typically these flares tend to resolve with time and appropriate nonsurgical treatment. As the arthritis progresses, the pain tends to worsen both in intensity and duration. In the later stages of the disease, the pain can be disabling.
Arthritic pain tends to “mechanical,” i.e. it is worse physical activities such as walking or work. Discomfort also occurs with specific activities such as getting in and out of a car, putting on shoes and socks/stockings and sitting in low chairs. Rest usually helps settle the pain.
Other symptoms of hip arthritis include stiffness typically in the morning and after prolonged sitting. Range of movement is generally lost especially moving the leg and to the side and backwards. As motion is lost, the spine is strained, leading to back pain.
Hip arthritis diagnosis