Patellofemoral Instability
The patella or kneecap is a small oval bone that is part of the extensor mechanism of the knee.
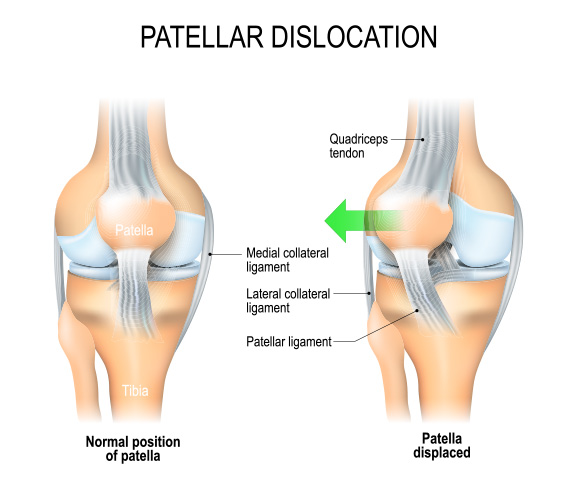
The patellofemoral joint (PFJ) comprises the patella and the end of the femur. With knee movement, the kneecap slides in a femoral groove (the trochlear). The quadriceps muscles are attached above via the quadriceps tendon. At the lower end, the patellar tendon attaches it to the tibia bone. The function of the patella is to enhance quadriceps strength. It also protects the knee from to some extent from a front on direct knock

Dislocation of the patella
Dislocation of the patella is a moderately common problem encountered with the knee. Stability of the patella is dependent on three main factors: 1. the conformity of the two bones; 2 the medial patellofemoral ligament (MPFL); and 3. the quadriceps muscles, especially the vastus medialis. When it contracts, the vastus medialis helps pull the patella in a medial direction.
When the patella dislocates, it pops out laterally or to the outside of the knee. It usually occurs with a twisting injury particularly with the femur twisting inwards. The dislocation can be a complete or partial (a so-called subluxation). The patella may either remain dislocated or spontaneously reduce. It can be often reduced immediately by gently straightening the leg. If it remains dislocated, it can be painful as the adjacent muscles often go into spasm. Sometimes the patella will be reduced at a Hospital Emergency Department.
Dr Brown has lectured on recurrent and acute patellofemoral dislocation, and has successfully treated many patients with this complaint.
Call us on (03) 5223 3151 Book an appointment today.