Shoulder Instability
The shoulder has an extensive range of movement at the cost of being an inherently unstable joint.
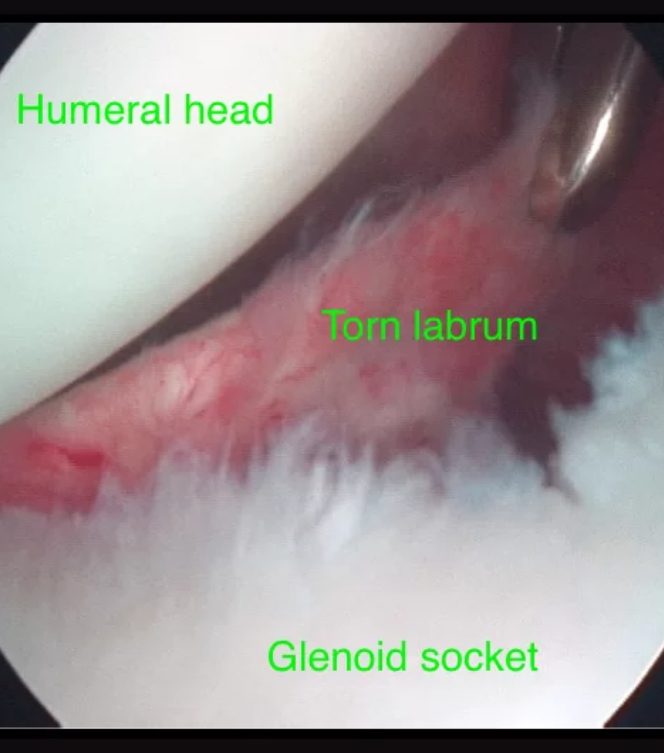
Often the bones of a joint contribute to its stability. But the shoulder has a mismatch between the size of the ball (humeral head) and the very shallow socket (glenoid). The glenoid labrum deepens the socket. The labrum is a fibrocartilage structure that sits around the circumference of the glenoid. As well as augmenting the glenoid, important strong ligaments are attached to it.
The main ligament that stabilises the shoulder is the inferior glenohumeral ligament. This ligament acts like a sling to support the head of the humerus. A group of muscles and tendons (the rotator cuff) also reinforces the shoulder. These muscles closely envelop the head of the humerus and are also important stabilisers of the shoulder.
There are a few patterns of shoulder instability. Anterior dislocations account for about 90% of shoulder dislocations. The shoulder can also dislocate posteriorly. There is even a group of people who have so-called multidirectional instability, i.e. it is unstable in all directions. Multidirectional instability can occur after many dislocations. However, it can also occur in people with a generally loose shoulder, and pain may be the biggest problem rather than laxity. Also, dislocations can be complete or partial (subluxations).
Dr Brown has successfully treated many patients with shoulder instability. After a thorough patient consultation, Dr Brown can recommend the most suitable non-surgical and surgical treatment to stabilise the shoulder.
Call us on (03) 5223 3151 Book an appointment today.
Anterior dislocation
As mentioned most shoulders dislocate anteriorly or out the front. It usually occurs in younger people playing sport. Typically the shoulder comes out when the arm is overhead and forced into external rotation. A dislocated shoulder causes immediate pain and loss of use of the arm. When looking at the shoulder, there is a characteristic deformity. Occasionally the shoulder reduces spontaneously. However, usually, the shoulder is manipulated in a Hospital Emergency Department after adequate pain relief and sedation. The patient uses a sling for comfort. Early movement is encouraged. Physiotherapy is helpful to facilitate this and also to help with a strengthening and rehabilitation program.
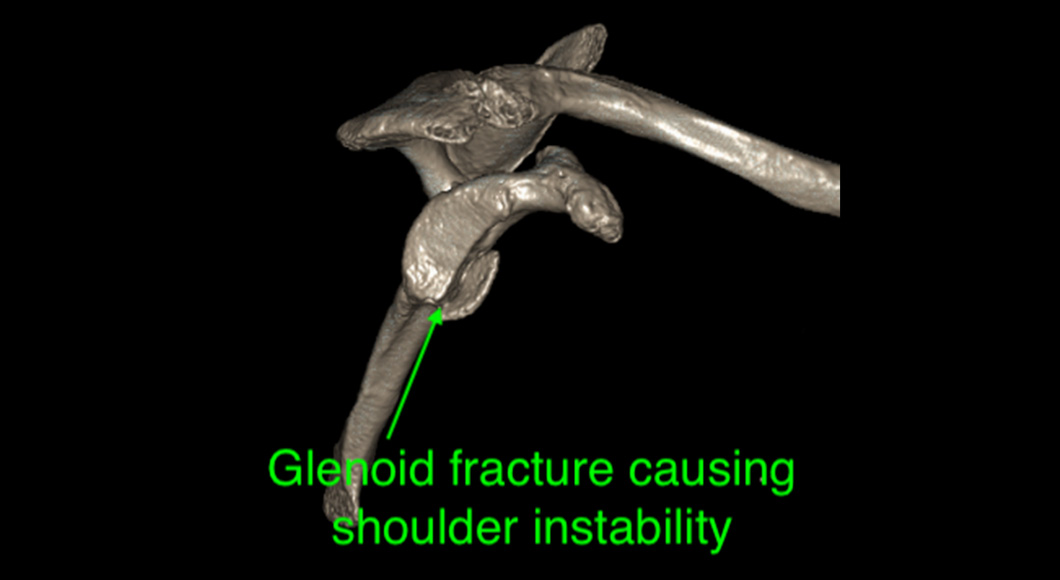
Anterior shoulder dislocations are a significant injury. Associated injuries are common. When the shoulder dislocates, the front and lower quadrant of the labrum tears away from the glenoid. This tearing is called a Bankart lesion and significantly contributes to the risk of further instability. Sometimes the glenoid bone is fractured in this region producing a bony Bankart lesion. When the ball dislocates, the back of it impacts onto the front of the socket, and an impaction fracture can occur, the so-called Hill-Sach’s lesion. The size of this bony defect can vary from a superficial dent to a significant divot in the ball.
Often the nerves around the shoulder are stretched. The nerve most at risk is the axillary nerve that innervates the deltoid muscle. Most injuries are mild and only associated with numbness over the outer part of the shoulder and mild weakness of the deltoid muscle. These typically resolve relatively quickly. Occasionally they can cause severe muscle weakness from which recovery can be slow. Rarely multiple nerves around the shoulder may be stretched, causing significant weakness of the shoulder and arm. Apart from glenoid fractures, sometimes the greater tuberosity (where tendons of the rotator cuff attach) is fractured. If these are widely separated, they may require surgical fixation. Rotator cuff tendon tears are common. Tears are common in persons older than 60 years but rarely occur in younger patients.
The most frequent outcome following a shoulder dislocation is the risk of recurrent episodes. This risk is directly related to the age when a person first dislocates their shoulder. The risk is as high as 80-90% for persons 18 years or younger. It decreases in older people with the risk of recurrence for persons over the age of sixty being only about 5%.
Treatment
The treatment for recurrent anterior dislocations is surgery. The primary cause for ongoing shoulder instability is a tear of the glenoid labrum. Arthroscopically it is repaired back to the bone. Commonly three to four small anchors are inserted into the bone, securely reattaching the labrum. It usually takes about three months for healing to take place. However, the person needs to wait six months before returning to contact sport. In conjunction with labral repair, often other procedures need to be performed according to what is else has been damaged.
If significant bone loss occurs, a more extensive procedure is required. Bone loss may be due to a large fragment of bone (bony Bankart), breaking away at the time of the initial dislocation. However, bone loss can occur after many dislocations. Bone loss from the shoulder ball exacerbates this problem. In this situation, stability cannot be restored with a soft tissue procedure as described above. A bone graft procedure is required. The bone graft of choice is to take a nearby bone, called the coracoid process, and transfer it to the front of the socket where the bone loss has occurred. Two screws hold the graft. This operation is known as the Latarjet procedure. The advantage of taking the coracoid is that a tendon (the conjoined tendon) remains attached to the bone and it also improves stability by acting as a dynamic sling. It also has a good blood supply that enhances healing.
Posterior Dislocation
Posterior dislocations are far less frequent. They usually occur with a fall onto the outstretched arm that drives the head of the humerus backwards. A posterior dislocation leads to tearing of the labrum from the back of the socket. Recurrent dislocations are less likely after a posterior dislocation.
Treatment
However, ongoing instability is managed by arthroscopic repair of the labrum.

Multidirectional instability
Often people with multidirectional instability suffer from generalised ligament laxity, and their shoulder instability is a manifestation of this. It also can occur in sports people like gymnasts and swimmers who put a lot of repetitive strain through their shoulders.
Treatment
Usually, the first line of treatment, if there has been no structural damage to the shoulder, is a thorough and extensive rehabilitation program. Rehabilitation involves a rotator cuff strengthening program and was well as strengthening the muscles that control the motion of the shoulder blade. Such a strategy needs to continue for at least six months. Avoidance of repetitive activities is necessary during this time.
For people who fail nonoperative treatment or if there is an underlying structural problem, they may require surgery. Typically the shoulder joint capsule and ligaments are stretched out. Arthroscopic surgery aims to “tighten” up the shoulder by placing multiple stitches through the capsule and in effect “double breasting” it. This operation is called a capsular plication. Postoperative rehabilitation again is extensive with the avoidance of aggravating activities for many months after.