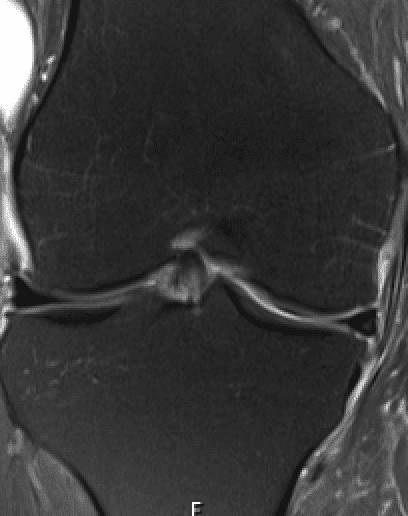
Magnetic resonance imaging (MRI) scans are widely used to help with the diagnosis of musculoskeletal pain. MRI uses a strong magnetic field and radio waves. The magnetic field works at the atomic level and forces protons in that body part to align with the magnetic field. These combine to create images of our joints in three planes to gain a three-dimensional representation of that particular body part. Unlike X-rays and CT scans, MRI scans don’t use potentially harmful radiation, so they are safe.
For the knee, an MRI defines all the major parts, including the ligaments, the menisci (shock absorbers), the lining of the joint, the articular cartilage and the bone, in incredible detail. It also shows the muscles, tendons, blood vessels, and nerves in great detail. For the shoulder, MRI produces excellent images of all the critical structures. Specifically, as well as the bone, cartilage and ligaments in all large joints, an MRI shows the glenoid labrum (important in shoulder dislocations) and the rotator cuff tendons.
The MRI scan is mainly interested in hydrogen atoms that are abundant in water and fat. Water accounts for about 60% of our body. When we injure our joints, often there is bleeding into the tissues, which is evident on an MRI scan. Later in the healing process, inflammation produces increased amounts of fluid in various tissues. In chronic conditions such as arthritis, there is also inflammation. The high water content in both situations will be evident on the MRI.
The detail that an MRI produces about the joint’s anatomy and the underlying disease process is truly unique. However, the MRI is so sensitive that it can easily “overcall” issues. For example, ACL tears are common; most athletes who tear their ACL will get an MRI scan. The ACL tear can be clearly seen, but in many cases, the scan will report a tear of other ligaments that may or may not be injured. It is the job of a radiologist to report the MRI findings. However, the orthopaedic surgeon’s job is to interpret the MRI and correlate the findings to the patient’s symptoms and examination findings to develop an overall diagnosis.
The same is true for chronic diseases. Often an MRI scan will demonstrate arthritic changes that may or may not correlate with the patient’s complaints or pain. An interesting study1 looked for the presence of knee arthritis on MRI scans in uninjured adults who had no knee symptoms, i.e. people who considered themselves to have normal knees for all intents and purposes. The results of the study were fascinating. The overall chance someone will have any osteoarthritic sign was 4-14% for those under 40 years old and 19-43% for those over 40 years. It also showed that the chance of meniscal tears is 10% overall, 4% for those under 40 but 19% for those over 40 years. The implication of this study is that the MRI is great at picking up arthritic changes, but these changes do not always correlate with a person’s symptoms or lack thereof. Again the MRI changes need to be interpreted by the treating doctor and not just taken at face value.
I see some patients who are totally freaked out by their MRI reports. The report’s conclusion may list many changes and show a myriad of pathology. Many of these MRI findings are not relevant. But, again, it is my job to interpret the findings in line with the person’s symptoms and physical findings. I often spend part of a consultation reassuring someone that their knee or shoulder is not as bad as the MRI thinks.
- Prevalence of knee osteoarthritis features on magnetic resonance imaging in asymptomatic uninjured adults: a systematic review and meta-analysis. Culvenor AG et al. British Journal of Sports Medicine, 2018. 1268-1278
For more information on how to book a consultation with Dr. Brown, please visit our Appointment page.